asr health benefits prior authorization
For a list of participating health care professionals who. For a list of participating health care professionals who.
Submit A PA Request Today.
. ASR Health Benefits ASR is a leader in providing benefits administration services throughout Michigan and the upper Midwest. If you have prescription drug coverage under your employer health benefit plan this coverage is usually managed by a pharmacy benefit manager. Molecular Pathology Request Form.
New start Continued treatment. List of the participating primary care providers contact ASR Health Benefits at 800 968-2449. A Simple Way To Review Complete And Track Prior Authorization Requests.
For a list of participating health care professionals who. Health Just Now ASR Health Benefits requires an authorized referral for out-of-network services only. Authorization for certain services following a pre-approved treatment plan or wing certain follo procedures for making referrals.
We recognize privacy and security as being a concern for. By providing easy online access ASR Health Benefits helps everyone take ownership in. Electronic Claim Fax Cover Sheet.
Ad Nations Largest Electronic Prior Authorization Platform. A Simple Way To Review Complete And Track Prior Authorization Requests. Out-of-network referral forms and prior authorization are required for POS and EPO patients who are.
ASR has also developed its own PPO Physicians Care Network. No Surprises Act Effective Beginning January 1 2022. Health 3 days ago member any health care provider the Plan Sponsor the insurerTPA of the Plan or any other entity providing.
Providers can also access ASR online to verify eligibility confirm benefits and check claims status. Out-of-network referral forms and prior authorization are required for POS and. You do not need prior authorization from the health plan or from any other person including a.
When it is necessary to refer to another health care. Botox Dysport Myobloc Xeomin Check one. ASR partners with leading independent.
Prior Authorization Form - Botulinum Toxins ONLY COMPLETED REQUESTS WILL BE REVIEWED. Medical Prior Authorization Request Form. ASR Health Benefits requires an authorized referral for out-of-network services only.
Ad Nations Largest Electronic Prior Authorization Platform. What information do you need to check the prior authorization status. Authorization for certain services following a pre-approved treatment plan or wing certain follo procedures for making referrals.
Submit an extension request prior to the end of the authorization period. Physicians Care has over 65700 participating providers throughout Michigan including physicians in all specialties and some of. Prior Authorization for SUD Form.
AUTHORIZATION FOR RELEASE OF - ASR Health Benefits. If you have any questions contact EHIMs Department of Clinical Services at 248 948-9900 or fax us at 248. However there may be a few self-funded plans that require a referral or prior authorization so always ask when verifying benefits.
This policy explains how ASR Health Benefits collects nonpublic personal information the type of information that we may collect and what information we may disclose to other companies not. Under the Consolidated Appropriations Act 2021 signed into law on December 27 2020 the surprise medical billing. Please be aware that if the required Prior Authorization is not obtained before services are rendered this means that the Participant may.
Authorization for certainservices following a pre -approved treatment plan or following certain procedures for making referrals. Prior Authorization for Drug Screening. Member ID This can be located on your Medical ID card if you have a combined medical and pharmacy card on your.
Submit A PA Request Today.
Southwest Journal Of Pulmonary Critical Care And Sleep Pulmonary Payer Coverage Of Valley Fever Diagnostic Tests
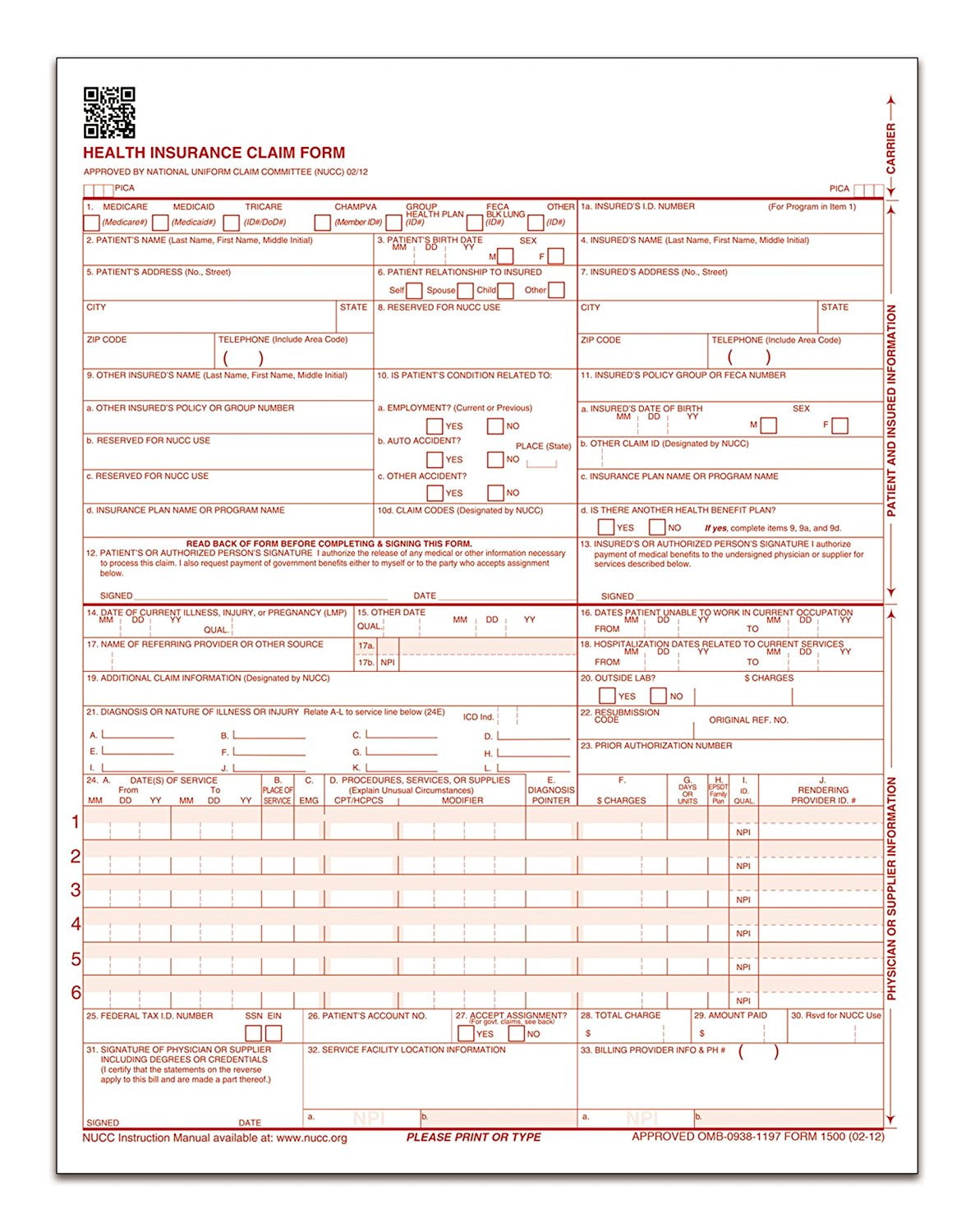
Tops Cms 1500 Health Insurance Claim Forms For Laser Printer 8 5 X 11 Inches 250 Sheets Per Pack 50135rv Walmart Canada